FAQ – Personalized iPS Cell Banking
When is the best time to bank iPSCs? Is there an age limit or minimum age for cell banking?
Generally is it advisable to bank iPSCs as soon as possible to ensure high quality of cell line and to preserve genetic and epigenetic integrity which provides a higher usability of cells for future applications.
There is no age limit or minimum for cell banking, however it is important to note that cell viability is lowered when aged.
What are iPSCs?
iPSCs are a type of stem cell that has the ability to renew itself indefinitely and be turned into any desired cell type in the body. Human iPSCs have properties that are similar to human embryonic stem cells, which are cells derived from the embryo that will eventually multiply and give rise to all cells in the body.
What is the difference between Stem cells and iPSCs?
Stem cells are undifferentiated cells that have the ability to differentiate into various specialised cells. Stem cells play an essential role in maintenance, repair and regeneration of tissues.
iPSCs on the other hand is derived from adult cells (blood cells or skin cells) that are reprogrammed in the lab and revert it back to pluripotent state similar to stem cells.
Both iPSCs and stem cells have been extensively studied for their therapeutic applications in regenerative medicine, where they can be used to replace damaged or diseased tissues.
How long can iPSCs be stored?
All iPSCs will be cryopreserved in Liquid Nitrogen. When cryopreserved, iPSCs can be stored for an extended period of time till the end of your service contract.
Can I still bank my iPSCs if I have other diseases?
Generally you can still bank iPSCs if you have other diseases, please contact us for further information
How much blood is needed from me?
Approximately 16 ml of blood is collected.
What is the process of iPSCs banking?
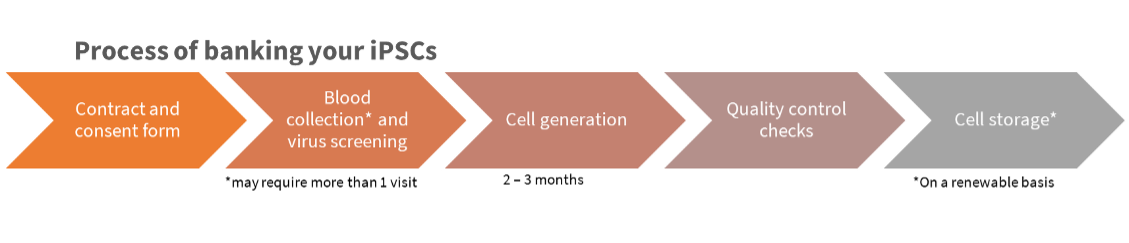
How long does the process take?
4-5 months (qc + banking)
How are iPSCs programmed?
iPSCs are generated through introducing specific transcription factors such as vectors and small molecules into adult cells such as skin or blood as they are generally less invasive. After which, the cells are cultured under specific culture media that promotes the transition to pluripotent state to increase the survival and proliferation of pluripotent stem cells. Over time, the cells are validated to confirm their pluripotency through expression markers and evaluate their ability to differentiate. Once validated, cells will be cryopreserved.
Can other people use my iPSCs?
No. Other people cannot use your personalised iPSCs as your cells might be a mismatch in the genetic makeup, increasing the chances of immune rejection.
What can the iPSCs be used for and what kind of disease can iPSCs treat?
Human iPSC research is advancing rapidly and there is unlimited potential for these cells due to their ability to be converted into any cell type of the body.
Human iPSCs can generate pancreatic islet cells, neuronal cells, immune cells, mesenchymal stem cells, cardiac cells, retinal cells and many others. The relevant cell types may be used to address various human disease conditions including diabetes, blood cancers and disorders, macular degeneration and retinal disease, Parkinson’s disease, spinal cord injury, ischaemic heart disease and more.
How much does it cost to bank my cells?
Please reach out to us
Are there any risks involved?
While iPSCs hold a significant promise for regenerative medicine, there are risks involved as well.
Some of the risks include increased risk of tumorigenicity due to the pluripotent nature of iPSCs, leading to uncontrolled growth and differentiation. In addition there might be Off- Target Effect of Gene Editing leading to undesirable genetic modification leading to unpredictable consequences of safety and efficacy of iPSCs
What mechanisms are put in place for the protection of my privacy and confidentiality?
Protection of privacy and confidentiality is paramount to us. Several mechanisms are put in place to safeguard the privacy and security of donors. All donors are provided with detailed information about the purpose and risks of the procedure. Informed consent forms will be given to donors where it will outline how donor information will be collected, used and protected. Donors have the right to withdraw their consent at any time point.
Donor’s information, including name and address are replaced with unique codes to anonymise samples and data, preventing the identification of individuals.
Researchers and clinical advisors involved are required to sign confidentiality agreements outlining their obligations to protect the confidentiality of donor information.